“The National Pressure Ulcer Advisory Panel serves as the authoritative voice for improved patient outcomes in pressure ulcer prevention and treatment through public policy, education and research.”
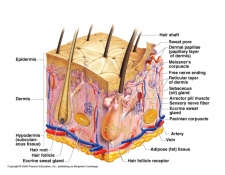
The International NPUAP-EPUAP defines pressure ulcer as a “localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear. A number of contributing or confounding factors are also associated with pressure ulcers; the significance of these factors is yet to be elucidated.”
Pressure ulcers or bedsores, are injuries to skin and underlying tissues that result from prolonged pressure on the skin. The development of pressure ulcers most commonly occur on bony areas of the body, such as the heel, ankles, hips, head or buttocks. Individuals who are confined to a bed for prolonged periods, required to use a wheelchair, or have a medical condition that limits them from easily changing positions are the most susceptible to developing pressure ulcers. According to the Mayo Clinic “bedsores can develop quickly and are often difficult to treat.” There are several strategies that can help prevent some bedsores and promote healing.
The NPUAP has categorized and defined (listed below) bedsores into four stages based on their severity. The severity of the pressure ulcer is ranked from stage I, the beginning stage, to stage IV, the most severe, where the ulcer exhibits large-scale tissue loss.
Category/Stage I: Non-Blanchable erythema
Skin is intact with non-blanchable redness (lighter color skin) or darkly pigmented skin may not have visible blanching of a localized area usually over a bony prominence. “The area may be painful, firm, soft, warmer or cooler as compared to adjacent tissue.”
Category/Stage II: Partial thickness
Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough or bruising.
Category/Stage III: Full thickness skin loss
Full thickness tissue loss, bone, tendon and muscle are not exposed but subcutaneous (adipose tissue) fat may be visible. The depth of the ulcer can vary depending on the amount of subcutaneous tissue present in the region.
Category/Stage IV: Full thickness tissue loss
The most severe stage, full thickness tissue loss with exposed bone, tendon or muscle has occurred.
Common sites of pressure ulcers for people who use a wheelchair develop on the tailbone, shoulder blade, spine, back of arms and legs where they rest against the chair. People confined to beds often develop pressure ulcers on the back or sides of head, rim of the ears, shoulders or shoulder blades, hip, lower back, tailbone, heels, ankles and the skin behind the knees.
Risk factors for developing pressure ulcers include anyone with limited mobility and is unable to easily change positions while seated or in a bed. Immobility may be due to:
- Generally poor health or weakness
- Paralysis
- Injury or illness that requires bed rest or wheelchair use
- Recovery after surgery
- Sedation (surgical procedure)
- Coma
Relieving pressure from the pressure ulcer site is the first step in treatment. The use of support surfaces (special cushions or pads, mattresses and beds) and patient repositioning can help reduce the pressure on the sore. There are a whole host of treatment options that are available to people with bedsores or pressure ulcers that are out of the scope of this post, so please feel free to visit the NPUAP site for more resources.
The impact of pressure ulcers upon patients and families can be traumatic and life changing, so please help spread the word to help increase awareness of this global challenge that health care providers face on a daily basis. For further information about National Pressure Ulcer Advisory Panel and pressure ulcers please visit: NPUAP
Leave a Reply