How Have Microorganisms and Bioburden Been Measured?
In the previous blog post regarding X-Ray lead aprons, we explored the history of healthcare associated infections or HAIs, and how transmission risks are posed to patients and staff via contaminated “high touch, non-critical surfaces,” including X-Ray aprons and protective lead wearables. In laying out the content of this blog, I was reminded of the phrases, “things aren’t always as they appear” and “don’t judge a book by its cover.” Is it possible that newer (clean looking) X-Ray aprons can carry a higher level of biological contamination when tested in comparison to older X-Ray aprons (which are dirty looking & smelling)? It is completely possible and plausible due to the concept of bioburden.
What is Bioburden?
Bioburden is defined in numerous medical dictionaries as the number of microorganisms contaminating an object. So how does one assess for bioburden? The gold standard for assessing for bacterial/fungal contamination has been to assess for colony forming units or CFUs. A CFU equals one viable bacterium that has the ability to spread and replicate.
3 Main Ways to Measure CFUs:
- A scientist could dilute the sample and count the bacteria by microscopic examination or through the use of a cell counter. However, if bacteria are too small or clump together, then this method is problematic. This method will yield total bacteria counts, both living and dead.
- A scientist could use Optical Density (OD) to estimate the number of viable bacteria in a sample. This is where the scientist measures how cloudy a liquid culture of bacteria is. While the bacteria are actively growing the liquid culture should continually become more and more cloudy. Again, this method will yield total bacteria counts, both living and dead.
- A scientist could make serial dilutions of a liquid culture and plate out the bacteria in known dilutions until they can count single colonies and extrapolate back to figure out total CFU in a sample. This method only yields viable bacteria totals.
4 Challenges Associated with Bioburden Assessment
Assessing for bioburden (microorganisms) by calculating CFUs is not as easy or straight forward as one might imagine.
- The first challenge posed is that one needs to have a lab in which to grow bacteria, and depending on the bacteria one is dealing with there are different governmental regulations to follow.
- The second challenge presented is that of time, one needs to have the time and equipment to properly grow the bacteria/fungus. Different species of bacteria or fungus grow at different rates, for example, culturing of bacteria on plates can take anywhere from overnight to multiple days.
- A third and very important challenge is posed by the bacteria and fungus themselves. They are similar to people in the fact that not all of them grow and thrive under the same conditions. In lab work, if only one kind of food source is used, one will only be able to assess for bacteria that grow on that particular food source.
- Finally, one needs to have a trained technician who knows how to assess which bacteria to grow under the correct conditions and then also how to properly count the bacteria.
While assessing for CFUs has traditionally been viewed as the gold standard for assessing bioburden, and it is vitally important for various microbial studies, it is not a good way to assess bioburden in real time. It can be complicated.
What is ATP and How is it Evaluated?
What if there was an easier way to determine surface levels of biological contamination?
What if there was an easier way to assess for a molecule that is found only in living cells, both bacterial and human living cells?
There IS an easier way to evaluate for this molecule in real time (by using a simple swab and handheld reader), and it can be used by any hospital staff member as a surrogate for such complicated CFU work. Let me introduce you to the molecule known as the “molecular workhorse,” called adenosine triphosphate (ATP).
Adenosine Triphosphate (ATP)
ATP is an energy molecule utilized by cells. It is present in humans, animals, plants and microbial cells. ATP levels rise as a cell is undergoing apoptosis (programed cell death), but is generally consider to be completely degraded within 30 minutes of cell death (1). This makes ATP a useful marker for the presence of unwanted biological contamination, including organisms that can cause infection and disease.
Okay – Get to the Point!
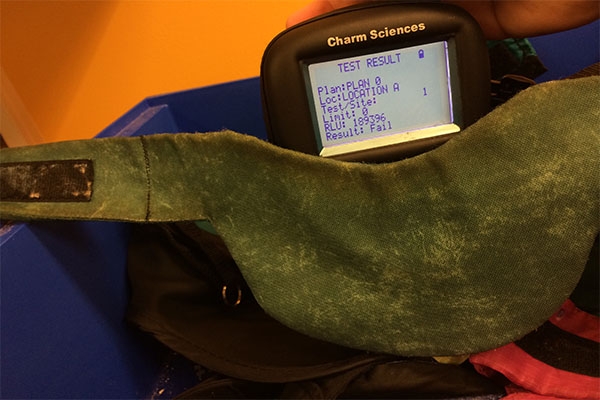
An increase in biological cells on a surface results in an increase in the amount of ATP present on that surface, thus making ATP an effective marker for the assessment of the hygienic status of an environmental surface. Simply stated, the amount of ATP present on a testing swab is a quantitative measurement of the cleanliness of the surface tested! In fact, ATP cell viability assays were determined to be the fastest, most sensitive, and least prone to artifacts, partially due to a lack of an incubation period (2). The sensitivity of laboratory cell based ATP cell viability assays can detect fewer than 10 cells per well (2). This technology has been modified to create a portable, ATP bioluminescence test, using a swab instead of plated cells. This now allows for a real time assessment of bioburden on site. These tests have been used to assess bioburden in many healthcare settings, including the ICU (3). ATP measuring units, called luminometers, are handheld, user friendly, and display the results in seconds. (It doesn’t take a scientist to use an ATP luminometer!) The read out of an ATP bioluminescence test is not in CFUs, but is in relative light units or RLUs. In the past, some scientists have questioned the validity of using a bioluminescence test instead of assaying for CFU.
Is There a Correlation Between CFUs & RLUs?
Like most assessments, ATP bioluminescence assays also have limitations, but they are an excellent surrogate that allows the everyday staff member to assess bioburden in real time. Those new to ATP bioluminescence testing often inquire about a correlation between CFUs and RLUs. (Most laboratory microbiologists have the capability to perform CFU testing, and are not confined to real time assessment of bioburden.) The most controlled way to achieve this is to look at different known amounts of CFUs and assess whether or not the RLUs increase accordingly. That is exactly what Dr. Sciortino’s group did when they assessed three different portable ATP bioluminescence kits for their ability to detect various CFUs of two different HAI relevant bacteria (Staphylococcus aureus and Acinetobacter baumannii) and one strain of fungus (Candida albicans).
What they discovered was there was a linear relationship between bacterial CFUs and RLUs for all three luminescence kits, and for two of the three kits between fungal CFUs and RLUs (1). Such research validates that the use of ATP luminometers can be used to assess for bioburden on surfaces in real time. This research, plus Dr. Jaber’s study, in which 25 lead aprons were cultured for CFUs and showed that 21 were colonized with Tinea species (the family of fungus that causes ringworm) and 21 were colonized with Staphylococcus aureus, of which 3 aprons were colonized with MRSA (4), validates the ATP bioluminescence results for X-ray aprons and protective lead wearables.
In fact, these X-ray aprons and protective lead wearables, which are worn throughout many different areas within a healthcare system, including the operating rooms, cath labs, radiology/imaging areas, emergency rooms and beyond are regularly testing with RLU readings in the THOUSANDS to HUNDREDS OF THOUSANDS (5), which is scary. The bottom line is regardless if you are a classically trained microbiologist used to looking at CFUs or a hospital staffer looking at luminometer readouts in RLUs, when surfaces inside an OR or Cath Lab are testing in the hundreds of thousands range, it is a problem!
Is ATP Testing Growing in Use?
Through utilization of ATP luminometer testing systems, companies like Radiological Care Services (Indianapolis) are able to enter a facility’s Cath Lab, OR or Radiology Department and test lead apron inventories on site, providing real time numbers (bioburden levels) in a matter of seconds. An advocate for ATP luminometer testing, Dr. Sciortino even states, “ATP system monitoring may uncover the need for new disinfectant designs that adequately remove hospital surface biofilms, rendering used hospital equipment to its native state whereby a zero reading by ATP monitoring can be achieved” (1). If you look back at the first blog post, “Contaminated X-Ray Aprons and The Risk of HAIs”, I positioned that “using wipes alone” was insufficient and through the use of ATP testing, Dr. Sciortino could be inferring a similar position.
Looking Ahead…
In the next blog post, we’ll specifically look at the science/methodology behind the use of sanitizing wipes and we’ll further explore the differences between true “cleaning” and “sanitization.” We’ll later examine what the governing bodies, such as AORN, CDC, HFAP and JCAHO state regarding their expectations of such surfaces within healthcare facilities. Understanding the science behind HAIs, testing for biological contaminants on surfaces, biofilms, and the difference between “cleaning” and “sanitization” will help us understand that current healthcare protocols in regards “non-critical, high touch surfaces” need to be changed in order to better protect hospital patients and staff.
About The Author:
Kathleen R. Jones received her BS from Purdue University (West Lafayette) in Biology specializing in Genetics and Microbiology. After working for five years in Quality Control she then completed her MS at Purdue University in Indianapolis. Her growing interest in Infectious Diseases lead her to the Uniformed Services University of the Health Sciences where she obtained a Doctorate in Emerging Infectious Diseases. Kathleen has a passion for progressive sciences and initiatives, and employs her keen understanding of the biofilm formation and elimination processes into her research and work.
Sources:
- Sciortino, C. V. and R. A. Giles. 2012. Validation and comparison of three adenosine triphosphate luminometers for monitoring hospital surface sanitization: A Rosetta Stone for adenosine triphosphate testing. AJIC. 40 (e233-9)
- Riss T.L., R.A. Moravec, A. L. Niles, H.A. Benink, T.J. Worzella, L. Minor. Minor, L, editor. 2013, Cell Vialblity Assays. In: Sittampalam G.S., N.P. Coussens, H. Nelson, et al., editors. Assay Guidance Manual [Internet]. Bethesda (MD): Eli Lilly & Company and the National Center for Advancing Translational Sciences; 2004-. Available from: //www.ncbi.nlm.nih.gov/books/NBK144065/
- Moore, G., D. Smyth, J. Singleton, P. Wilson. 2010. The use of adenosine triphosphate bioluminescence to assess the efficacy of a modified cleaning program implemented within an intensive care setting. AJIC. 38(8):617-622 DOI: //dx.doi.org/10.1016/j.ajic.2010.02.011
- Jaber, M., M. Harvill, E. Qiao. 2014. Lead aprons worn by interventional radiologists contain pathogenic organisms including MRSA and tinea species. Journal of Vascular and Interventional Radiology. 25:3:S99-S100. DOI: //dx.doi.org/10.1016/j.jvir.2013.12.279
- “Outcomes: What do your numbers look like?” Radiological Care Services. Nov 20, 2014. //www.radcareservices.com/radiolgical-care-services-outcomes.html
Thank you for sharing your experiences with us Dr. Sieber! I can’t tell you the number of customers and blog subscribers that have inquired about proper lead apron cleaning practices. Given the amount of inquires we have collectively received, there is clearly a need for more definitive requirements and recommendations regarding the cleaning and testing of lead wearables. I couldn’t agree with you more regarding the need for “national change” in requirements and recommendations.
It is our goal with these guest blog posts to help raise awareness of how medical professionals and facilities can test the hygienic status of their lead wearables by using ATP testing. Once again, thank you for taking the time to share your experiences with us here on the blog! Hopefully, we can keep the discussion going and gain additional insights from other medical professionals. Please share this post with your colleagues.
What an insightful blog entry to have been copied on – Thank you for sharing this insight into how ATP Bioluminescence works. In having worn lead aprons in the operating room for 20+ years, I can assure you, they are (for the most part) rather disgusting! They have grossed me out and bothered me for years. They are routinely covered in sweat, blood, casting materials, surgical debris and more…and rarely are they ever cleaned/serviced/taken care of. I will be clear not to “point fingers” at anyone (hospital system, title, position, etc.) for failure to do so, it simply has “slipped under the radar” it seems for the past several years. I have colleagues across the United States that I have posed this question to and most agree that their facilities do little (or nothing) to properly clean and take care of these garments. This is not a “hospital specific” issue per se, but a broad based issue that needs to be addressed as a Nation. A few friends shared with me that they had seen a few staff members try and use a sanitizing wipe to clean the aprons with, but I can assure you, this will not adequately remove the layers of biofilm…they need to be cleaned and sanitized. I find it rather frustrating that groups such as JCAHO, HFAP and AORN have requirements and recommendations for many items and surfaces inside of the operating room, yet they don’t make a specific requirement of lead aprons? So it is important to monitor the sides of a kick bucket or the straps on a table, but nothing is needed for an apron that is not only worn inside of the OR, but then around other parts of the hospital too? This is not good for patient safety at all. National change is needed on this issue and ATP testing could be very helpful and used to help monitor the status of these garments.