Main Content
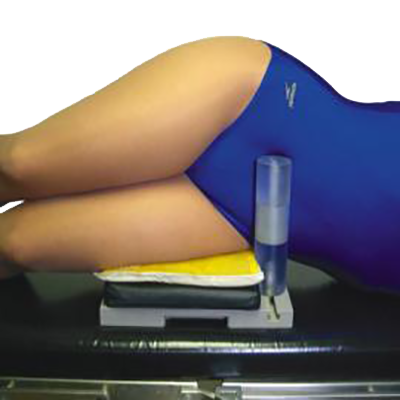
We'll Help You Select the Right Lead Apron.
Choosing the right lead apron for your radiation protection needs is our most popular request. We're here to help.
Find the Leading Medical Products for Your Institution or Practice
Our easy-to-use, secure e-commerce site includes in-depth information and pricing on products for hospitals, medical and surgical practices, dentists, vetinarians, imaging centers, and laboratories. You're just a few clicks away from having our quote for the items you need today.